Sustaining diabetes self-management programs: Community members speak
Ideas flowed at a conference on maintaining the benefits of a community health program, writes Anne Renz
by Anne Renz, MPH, Group Health Research Institute (GHRI) project manager
Diabetes is a significant public health concern, affecting 640,000 Washingtonians and leading to $3.75 billion annually in direct medical expenditures (as of 2012).1 Self-care workshops can help mitigate this public health issue. In 2013, GHRI Senior Investigator Katherine Newton, PhD, received a grant to implement these workshops in underserved communities. I’ve been on the research team for this project for the past 18 months.
Of course, when a community-based program is started with research money, an immediate question is, “How can the program remain sustainable after the startup grant funding ends?” This is a question we have been asking ourselves and others for the past three years. Our project to implement Diabetes Self-Management workshops in English and Spanish has built up a cadre of master trainers and lay leaders, as well as community connections for recruiting participants and hosting workshops. Hundreds of people, mostly lower-income Central and Eastern Washington residents, have gained self-confidence and actionable skills to better manage their diabetes. As the final six months of funding approach, we have further focused our efforts on addressing sustainability.
To that end, in April, we hosted an invitational sustainability conference at Central Washington University in Ellensburg. We brought together a diverse group of stakeholders to explore strategies for sustaining diabetes and other self-management programs at the state and local level. Our planning committee guided topic development and identified key stakeholders across the state.
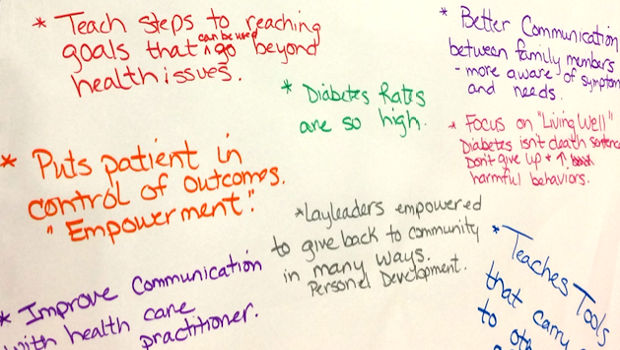
The World Café encourages everyone to get their ideas on the table
We considered how best to solicit and record ideas from attendees and stakeholders in a half-day conference. Based on suggestions from planning committee member Deb Miller and enthusiasm from the rest of the committee, we selected the World Café method as the means of gleaning information. This approach is centered on asking powerful questions and getting broad input to their answers through conversation and dialogue. "Hosts" record and then share the key points from conversations at their table. The goal is to reap a rich landscape of ideas, rather than narrowing down to a few next steps.
We were fortunate to have many key stakeholders at our conference, motivated only by their goodwill and the promise of a boxed lunch. Attendees included directors and project managers from our four funded sites (Community Choice in Wenatchee, Benton-Franklin Health District in the Tri-Cities area, Inland Northwest Health Services in Spokane, and Grays Harbor County Public Health in Aberdeen). In addition to those already participating in our programs, we invited stakeholders from businesses, employers, insurers, the state Department of Health, community-based organizations, and clinics, as well as diabetes researchers, Diabetes Self-Management Program (DSMP) lay leaders, and community health workers.
Communities and businesses benefit from diabetes self-management
The opening presenters shared state-level, lay-leader, and employer perspectives. On the state level, diabetes has a major impact on health care costs and the well-being of residents. The DSMP is one way to address the challenges of diabetes. Our lay-leader speakers shared examples of the community impact of the program, including moving testimonial videos of workshop participants. Lastly, a representative from First Fruits of Washington and Vista Hermosa (their foundation) shared their philosophy and business case for offering DSMP workshops as an investment in their employees' well-being. As the representative said, healthy employees are productive employees.
The conference tapped into the practical resources and wealth of knowledge held by community stakeholders. When we summarized the presentation and table host notes, they filled 10 pages. The findings underscored the wider impact of self-management skills in creating healthy communities. Attendees defined health benefits broadly, including improved individual habits, family communication, intergenerational patterns, and professional development for lay leaders. They stated the importance of making a business case to potential funders (Ask “How much does it cost not to do it?”) and moving them with testimonials (“Make them cry”). The conference showed the breadth and depth of support for the workshops, was a tremendous reminder of the wider impact of diabetes on community health, and was a unique opportunity to gather the creative power of community stakeholders. This energy now must be channeled into specific funding and sustainability strategies. We’re continuing our regularly scheduled calls with the project sites. They’ll be giving us updates, sharing their ideas, and giving and receiving feedback on their work. We look forward to helping them over the next several months in supporting diabetes self-care in their communities.
1 Diabetes Epidemic & Action Report (PDF, 3.2M). Washington State. 2014.