The world seems unstable but are there some constants in health?

Dr. Eric B. Larson sees parallels between personal resilience and sustainable, quality health systems.
by Eric B. Larson, MD, MPH, Group Health Research Institute (GHRI) executive director, and Group Health vice president for research
If you follow current events, you might be feeling unsettled. I was in the United Kingdom right after the Brexit vote to leave the European Union. I returned home during our major political party conventions. The daily news reports conveyed uncertainty, but to my surprise, when I returned from my travels, I felt a reassuring sense of stability. How could this be, given the crazed political season we’re in?
My outlook stems from a Lancet Commission meeting I attended in London. The purpose of the meeting was to produce a review of dementia, including Alzheimer’s disease. I took a chance and proposed to my collaborators that we include resilience in our comprehensive report. In the context of dementia research, resilience means adapting to age-related brain changes. It means having cognitive function at age 90 and beyond, when most people have dementia. Somewhat to my surprise, my colleagues embraced my suggestion. Our review will include a section describing how our long-running Adult Changes in Thought (ACT) study found that some very old people with pathologic changes of Alzheimer’s disease on autopsy such as brain plaques and tangles, did not show cognitive decline before they died. ACT is now studying the genetic, behavioral, and environmental factors that make some people resilient against late-life dementia.
Taking the long view about health and health care
One possible key to resilience is taking the long view about personal health—making physical activity, good nutrition, and an active social life part of your everyday routine. Another healthy practice we can develop over time is self-awareness, meaning understanding ourselves well enough to know when a cold, back pain, or headache will probably resolve with a little time. Coming to this awareness means knowing that this is how humans are built. Homeostasis, or the tendency to remain stable through constant physiological adjustments, is our natural condition. With time and experience, we can get a sense of when a health change might be serious and when a new symptom might resolve without treatment.
A recent conversation with a friend at the University of Washington made me think about the value of taking the long view about health care. Over coffee, we talked about a 2001 article that was a reprise of a classic 1961 paper on the ecology of medical care. In this case, ecology means the relationship between people and the medical system. The bottom line of both studies is that in health care, some factors remain constant. If we pay attention to these factors, we can structure our health care systems for long-term resilience.
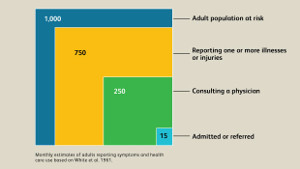
Both the 1961 and the 2001 papers used a clever framework. They used data on symptoms and health care use to create averages of how 1000 people use health care over one month. You might expect dramatic differences from the 1960s to the 2000s because of changes such as the introduction of Medicare, Medicaid, and new treatments. However, the striking finding for me was that some basics of medical care—how many people seek it and where they go to get it—are stable. In both studies, in one month, 75 to 80 percent of people had symptoms. Of these, 33 percent in one study and 42 percent in the other consulted a physician, most in primary care rather than a hospital.
Since I’ve been thinking about what makes people personally resilient, I noticed that fewer than half of the people estimated to have symptoms in a month contacted a doctor. In the United States, access and cost could affect that number. But the 1961 paper used data from both the United States and England and Wales, which have a national health service.
Good health care supports resilience
This brings us back to system resilience. A good health care system supports us in self-awareness about our health. Group Health, for instance, provides members with evidence-based information, in plain language, about conditions from chest pain to diabetes. Our nurse consulting service, available by telephone or secure online messaging, helps members decide when watchful waiting is the best course and when our symptoms might need medical attention. Group Health aims to promote resilience and especially, enlightened self-care.
So in this environment where every news story seems to bring a new worry, remember resilience. Think about how you can cultivate it and learn to increase your self-sufficiency. Build healthy habits and self-knowledge and rely on your health care system when you need it.
Please watch for our review of dementia in The Lancet. ACT and other GHRI studies will continue to work on the best ways to support you in making wise decisions about your health.